AMH Conversion Calculator and Guide
AMH Conversion Calculator
Understanding AMH: A Simple Guide
As someone who’s always been fascinated by the intricacies of human biology, I recently dove into the topic of Anti-Müllerian Hormone (AMH) and its significance. If you’re curious about what AMH is and why it’s important, especially in the context of fertility and reproductive health, let’s break it down into simpler terms.
What is AMH?
AMH stands for Anti-Müllerian Hormone. It’s a protein hormone produced by cells in the ovaries. Think of AMH as a messenger that gives us insight into the ovarian reserve, which is essentially the number of eggs a woman has at any given time.
Why is AMH Important?
AMH levels are often discussed in relation to fertility. They are a helpful indicator of a woman’s ovarian reserve. This doesn’t predict the chances of becoming pregnant right away, but it gives a general idea of how many eggs are available for fertilization.
How is AMH Measured?
In the United States, AMH levels are typically measured through a blood test. Here’s how it works:
- Blood Sample Collection: A healthcare professional draws a small amount of blood, usually from your arm.
- Laboratory Analysis: This blood sample is then analyzed in a laboratory, where the AMH level is measured in nanograms per milliliter (ng/mL).
- Interpreting Results: Your healthcare provider will explain the results. High AMH levels might suggest conditions like Polycystic Ovary Syndrome (PCOS), while low levels could indicate a reduced ovarian reserve.
AMH Levels: What Do They Mean?
- High AMH Levels: May be seen in conditions like PCOS.
- Low AMH Levels: Can suggest a lower number of remaining eggs.
Remember, AMH levels are just one piece of the fertility puzzle. They should be considered along with other factors like age and overall health.
Normal AMH by Age
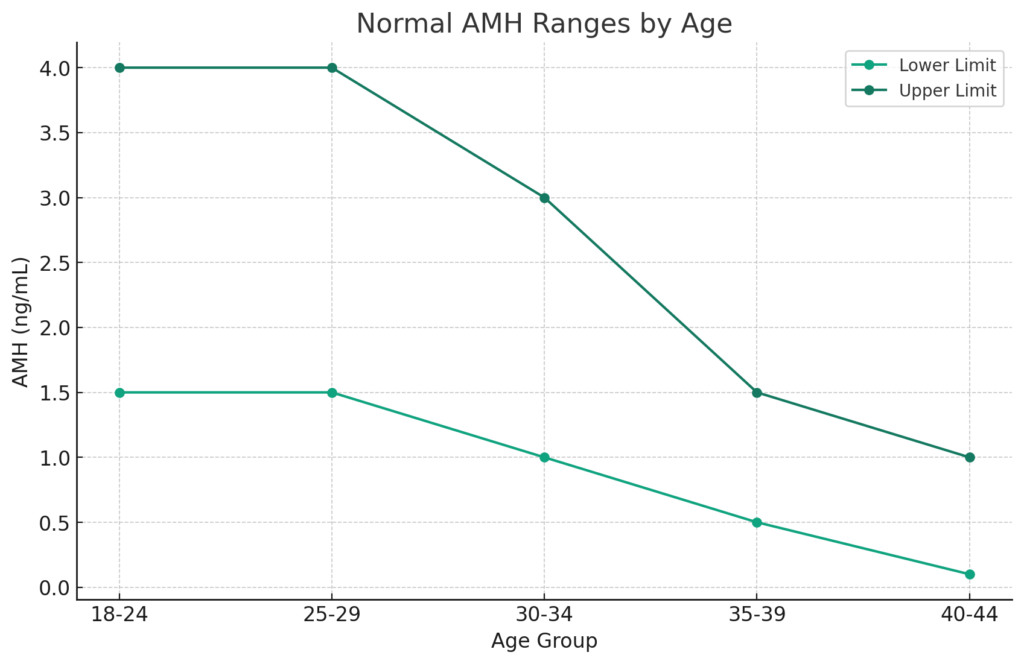
This chart illustrates the approximate normal ranges of Anti-Müllerian Hormone (AMH) by age group, measured in nanograms per milliliter (ng/mL). It represents general estimates and it’s important to note that these ranges can vary:
- Age 18-24: The AMH levels generally range between 1.5 and 4.0 ng/mL.
- Age 25-29: Similar to the 18-24 age group, the AMH levels typically range from 1.5 to 4.0 ng/mL.
- Age 30-34: Here, the range begins to lower slightly, with AMH levels ranging from 1.0 to 3.0 ng/mL.
- Age 35-39: The AMH levels further decrease, ranging from 0.5 to 1.5 ng/mL.
- Age 40-44: In this age group, the AMH levels are generally between 0.1 and 1.0 ng/mL.
Remember, these are approximate ranges and individual levels can vary. AMH levels are influenced by various factors, including but not limited to genetics and overall health. It’s always best to consult with healthcare professionals for personalized assessments.
AMH Conversion Table pmol/L to ng/mL
| AMH (ng/mL) | AMH (pmol/L) |
|---|---|
| 0.1 | 0.71 |
| 0.2 | 1.43 |
| 0.3 | 2.14 |
| 0.4 | 2.86 |
| 0.5 | 3.57 |
| 1.0 | 7.14 |
| 1.5 | 10.71 |
| 2.0 | 14.28 |
| 2.5 | 17.85 |
| 3.0 | 21.42 |
| 3.5 | 24.99 |
| 4.0 | 28.56 |
| 4.5 | 32.13 |
| 5.0 | 35.70 |
| 6.0 | 42.84 |
| 7.0 | 49.98 |
| 8.0 | 57.12 |
| 9.0 | 64.26 |
| 10.0 | 71.40 |
The Big Picture
Understanding AMH levels can be empowering, especially for women planning their future in terms of family and health. However, it’s important to approach this information as a single factor in a much larger picture of fertility and health.
If you’re considering getting your AMH levels tested or have already done so, remember that these numbers are not a definitive measure of your fertility potential. They’re simply a tool to better understand your reproductive health.
In conclusion, AMH is a fascinating hormone that offers valuable insights. As we continue to unravel the mysteries of the human body, it’s important to stay informed and proactive about our health. So, whether you’re deep into research about fertility or just starting to explore, I hope this simplification of AMH helps you on your journey!




Responses