What do Embryo Grades Mean? Your Guide to IVF Embryo Grading
Embryo grading in the IVF (In Vitro Fertilization) process is more than just a routine check; it’s a critical step that significantly influences the success of the journey towards parenthood.
Embryo grading is a combination of numbers and letters assigned by an embryologist that offers insight into the potential of each embryo to develop, implant, and grow. 4AA, 5AA, and 6AA are considered the best Embryo grades that are most likely to result in a live birth. Once an Embryo is confirmed Euploid grading has less importance.
Understanding embryo grades offers hopeful parents a clearer view of their IVF journey, guiding decisions and setting expectations. In this guide, we’ll simplify the complex world of embryo grading, explaining its importance in IVF and how it can shape the path to starting or growing a family.
Embryo Grading Systems
- The Gardner System: This is used specifically for blastocyst stage embryos (day 5 or 6 embryos). The Gardner system grades embryos based on three key aspects:
- The development stage of the blastocyst (numbered 1-6)
- The quality of the inner cell mass (ICM), graded as A (best), B, or C
- The quality of the trophectoderm (TE), the cells that will become the placenta, also graded as A (best), B, or C
- The Veeck System: This system is often used for grading day 3 embryos and looks at factors such as the number of cells the embryo has, the amount of fragmentation, and whether the cells are symmetrical.
- The grades usually range from Grade 1 (best) to Grade 4, with Grade 1 embryos showing even cell sizes, no fragmentation, and a clear cytoplasm.
Gardner Embryo Grading
The Gardner system is a detailed and widely used method for grading blastocyst-stage embryos during IVF treatments. It evaluates the embryos based on three main criteria: the degree of blastocyst expansion and hatching status, the appearance of the inner cell mass (ICM), and the appearance of the trophectoderm (TE).
What do the numbers mean in embryo grading?
The first part of the grading system, concerning the degree of blastocyst expansion and hatching status, uses numbers 1 through 6. Here’s what each number represents:
- Grade 1: Early blastocyst. The blastocoele (the fluid-filled cavity) is less than half the volume of the embryo.
- Grade 2: Blastocyst. The blastocoele is equal to or greater than half the volume of the embryo.
- Grade 3: Full blastocyst. The blastocoele completely fills the embryo, pushing the ICM and TE to thin the zona pellucida (the outer shell).
- Grade 4: Expanded blastocyst. The blastocyst increases in size and the zona pellucida thins to the point where hatching is imminent. The ICM and TE are clearly defined.
- Grade 5: Hatching blastocyst. The blastocyst begins to hatch out of the zona pellucida, starting the process of implantation into the uterine lining.
- Grade 6: Hatched blastocyst. The blastocyst has completely escaped from the zona pellucida and is ready for implantation.
What do the letters mean in embryo grading?
Following the numerical grade, the Gardner system also includes letter grades (A, B, C) to assess the quality of the ICM and TE, with ‘A’ representing the highest quality. For instance, a blastocyst graded as 5AA indicates a hatching blastocyst with both the inner cell mass and the trophectoderm being of the best quality.
The first number represents the quality of the inner cell mass (ICM), these are the cells that become the baby, graded as A (best) B, or C
The second number represents the quality of the trophectoderm (TE), the cells that will become the placenta, also graded as A (best), B, or C.
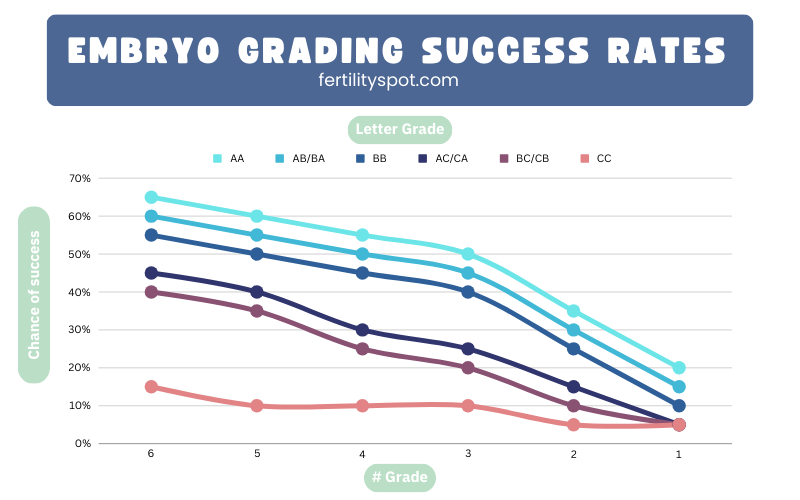
Chance of success by embryo grade
Providing success rates is very complex due to the variability based on numerous factors including individual clinic data, patient-specific factors, and embryo-handling techniques. However, I can provide a general table that reflects the typical trends in success rates based on the Gardner grading system for blastocysts. Please note that these percentages are illustrative and actual success rates can vary significantly:
| Embryo Grade | Description | Estimated Chance of Success* |
|---|---|---|
| 6AA | Hatched blastocyst, highest quality ICM and TE | High (~50-65%) |
| 6AB or 6BA | Hatched blastocyst, mixed quality ICM and TE | Moderate to High (~40-60%) |
| 6BB | Hatched blastocyst, good quality ICM and TE | Moderate (~35-55%) |
| 6AC or 6CA | Hatched blastocyst, high and lowest quality ICM/TE | Low to Moderate (~25-45%) |
| 6BC or 6CB | Hatched blastocyst, good and lowest quality ICM/TE | Low (~20-40%) |
| 6CC | Hatched blastocyst, lowest quality ICM and TE | Very Low (~5-15%) |
| 5AA | Hatching blastocyst, highest quality ICM and TE | High (~45-60%) |
| 5AB or 5BA | Hatching blastocyst, mixed quality ICM and TE | Moderate to High (~40-55%) |
| 5BB | Hatching blastocyst, good quality ICM and TE | Moderate (~30-50%) |
| 5AC or 5CA | Hatching blastocyst, high and lowest quality ICM/TE | Low to Moderate (~20-40%) |
| 5BC or 5CB | Hatching blastocyst, good and lowest quality ICM/TE | Low (~15-35%) |
| 5CC | Hatching blastocyst, lowest quality ICM and TE | Very Low (~5-10%) |
| 4AA | Expanded blastocyst, highest quality ICM and TE | High (~40-55%) |
| 4AB or 4BA | Expanded blastocyst, mixed quality ICM and TE | Moderate (~35-50%) |
| 4BB | Expanded blastocyst, good quality ICM and TE | Moderate to Low (~25-45%) |
| 4AC or 4CA | Expanded blastocyst, high and lowest quality ICM/TE | Low (~15-30%) |
| 4BC or 4CB | Expanded blastocyst, good and lowest quality ICM/TE | Low (~10-25%) |
| 4CC | Expanded blastocyst, lowest quality ICM and TE | Very Low (~5-10%) |
| 3AA | Full blastocyst, highest quality ICM and TE | Moderate (~35-50%) |
| 3AB or 3BA | Full blastocyst, mixed quality ICM and TE | Moderate (~30-45%) |
| 3BB | Full blastocyst, good quality ICM and TE | Low to Moderate (~20-40%) |
| 3AC or 3CA | Full blastocyst, high and lowest quality ICM/TE | Low (~10-25%) |
| 3BC or 3CB | Full blastocyst, good and lowest quality ICM/TE | Low (~5-20%) |
| 3CC | Full blastocyst, lowest quality ICM and TE | Very Low (~<5-10%) |
| 2AA | Blastocyst, highest quality ICM and TE | Low to Moderate (~20-35%) |
| 2AB or 2BA | Blastocyst, mixed quality ICM and TE | Low (~15-30%) |
| 2BB | Blastocyst, good quality ICM and TE | Low (~10-25%) |
| 2AC or 2CA | Blastocyst, high and lowest quality ICM/TE | Very Low (~5-15%) |
| 2BC or 2CB | Blastocyst, good and lowest quality ICM/TE | Very Low (~<5-10%) |
| 2CC | Blastocyst, lowest quality ICM and TE | Very Low (~<5%) |
| 1AA | Early blastocyst, highest quality ICM and TE | Low (~10-20%) |
| 1AB or 1BA | Early blastocyst, mixed quality ICM and TE | Very Low (~5-15%) |
| 1BB | Early blastocyst, good quality ICM and TE | Very Low (~5-10%) |
| 1AC or 1CA | Early blastocyst, high and lowest quality ICM/TE | Very Low (~<5%) |
| 1BC or 1CB | Early blastocyst, good and lowest quality ICM/TE | Very Low (~<5%) |
| 1CC | Early blastocyst, lowest quality ICM and TE | Very Low (~<5%) |
*These percentages are illustrative based on general trends and should not be used as definitive predictions of success. Actual success rates depend on individual circumstances, clinic practices, and many other factors.
Embryos graded with a ‘C’ for either the ICM or TE are generally considered to have a lower potential for successful implantation and pregnancy, but it’s important to remember that successful pregnancies can still occur with these embryos. Many sepecialists beleive that as soon as an embryo is considered a Euploid that the grading system no longer matters.
Conclusion
In conclusion, embryo grading, particularly within the framework of the Gardner system, plays a crucial role in the IVF process, offering invaluable insights into the potential viability and quality of embryos. While higher grades like 6AA or 5AA typically indicate a higher likelihood of successful implantation and pregnancy, it’s important to remember that embryos with lower grades or those marked with a ‘C’ also carry potential and have resulted in successful pregnancies.
However, it’s paramount to understand that embryo grading is just one piece of the complex puzzle of IVF. Success rates for each grade can vary based on a multitude of factors including individual patient characteristics, embryology lab protocols, and the specific practices of the fertility clinic. Therefore, these grades should be considered as guides rather than definitive predictors of success.
For individuals and couples navigating the IVF journey, open and informed discussions with fertility specialists are essential. These professionals can provide personalized insights, interpret the nuances of embryo grading in the context of your unique situation, and help manage expectations realistically.
In the journey towards creating new life, each step is delicate and profound. While embryo grading offers a scientific glimpse into the potential future of each embryo, the journey of IVF is a deeply personal and unique experience, shaped by the hopes, challenges, and the resilience of those embarking on this path to parenthood.




Responses